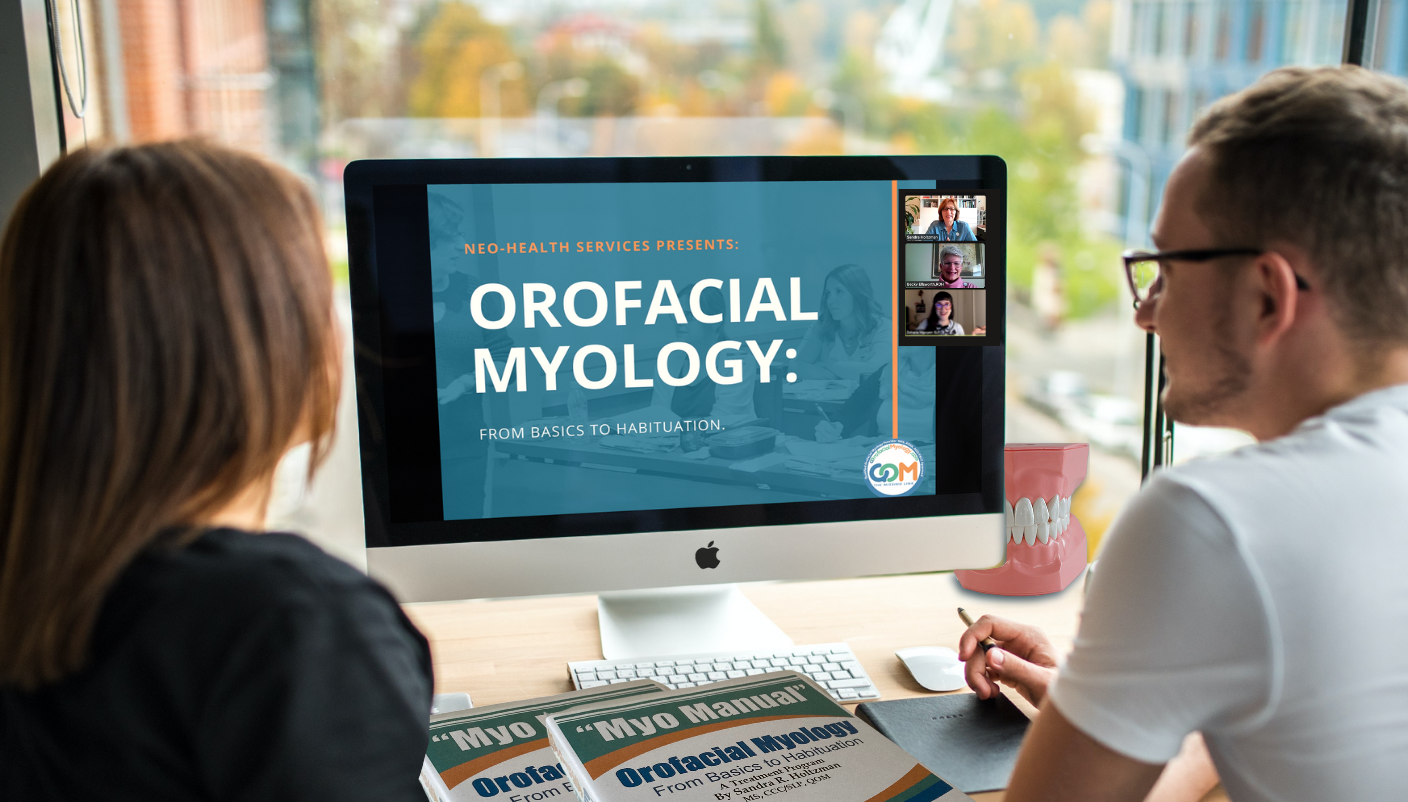

COURSE TESTIMONIALS
SLP
“The course is very well done in all aspects and now I really learned, unlike my last courses with others. I FINALLY found what I’ve been hoping for! Instructors explained excellently, ability to practice was amazing.”
RDH
"This was life-changing! The information was not only outstanding, but the presenters were also a huge part of making this course so enjoyable and exciting! I loved every minute!”
DDS
“This course truly is “the missing link”. As a pediatric dentist I can use and apply the knowledge I learned from this course to better serve my patients and to truly make a difference in their lives."
Click to explore 100s of Q&As
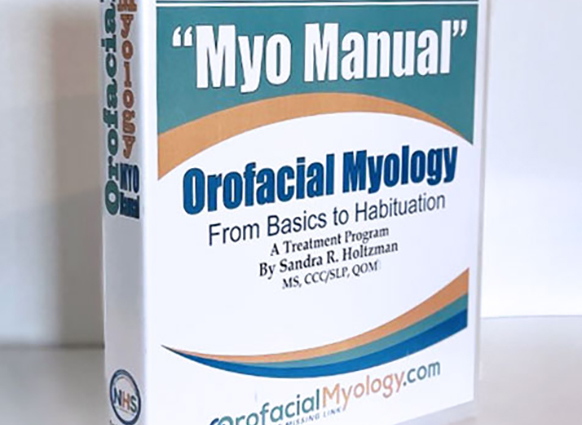
Orofacial Myology Tools
SEE THESE AND MORE...
-

 Add to cartMORE INFO
Add to cartMORE INFOBattle Buttons
$14.99Battle Buttons are used by the individual or with a “Battle Buddy” to improve lip closure, compression, strength, and resistance. Buttons and twine may be disinfected as needed. Colorful exercise buttons and sturdy twine make this a favorite of therapists and clients.
See Video
-

 Select options
Select optionsQuick Tongue Tie Assessment Tool
$7.49 – $54.99This disposable tool is used to perform a quick test for tongue-tie (ankyloglossia) as well as for general oral and facial measurements. Easy to use for right and left handed people. Measurements on both sides of tool. Directions are included in the package.
See Video
-

 Add to cartMORE INFO
Add to cartMORE INFO3 WAY MOUTH PROPS
$7.99The stabilization tool suitable for all your patients. Since mandibular involvement is such a common symptom of an oral myofunctional disorder, the clients are first given exercises to “dissociate” or separate mandibular from lingual movements. Prior to being able to achieve this, “assistance” is needed in the form of a 2-Way or 3-Way Mouth Prop to help the client achieve the desired goals of an exercise. The 3-Way Mouth Prop can be oriented as needed for each client.
See Video
-
 Add to cartMORE INFO
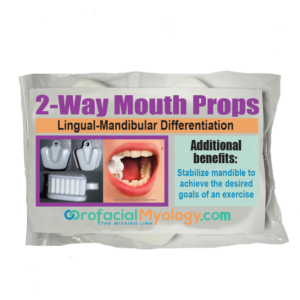
Add to cartMORE INFO2 WAY MOUTH PROP
$7.99The 2-Way Mouth Prop is a reusable stabilization tool. 2-Way Mouth Props (2WMP) can be oriented as needed for each client. Since mandibular involvement is such a common symptom of an oral myofunctional disorder, the clients are first given exercises to “dissociate” or separate mandibular from lingual movements. Prior to being able to achieve this, “assistance” is needed in the form of a 2-Way or 3-Way Mouth Prop to help the client achieve the desired goals of an exercise. Package of five props.
See Video
-

 Add to cartMORE INFO
Add to cartMORE INFOElevator Disks
$13.99Elevator Disks are colorful disks strung on sturdy cotton braiding. They are used to coordinate and improve lingual/labial/mandibular differentiation and labial competency, correct tongue placement on the alveolar ridge, and decrease hyper-gag. They are a favorite among clients of all ages.
See Video
-
 Select options
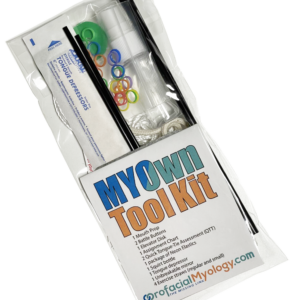
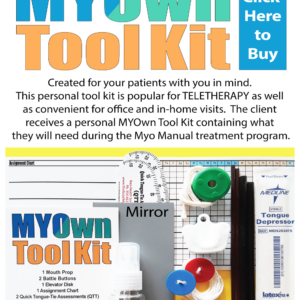
Select optionsMYOwn Tool Kit
$14.99 – $74.95This personal tool kit is popular for TELETHERAPY as well as convenient for office and in-home visits. The client receives a personal MYOwn Tool Kit containing what they will need during the Myo Manual treatment program.
The MYOwn Tool Kit includes: mouth prop, Battle Buttons (x2), Elevator Disk, assignment chart, Quick Tongue Tie Assessments (x2), Neon Elastics, squirt bottle, tongue depressor, mirror, exercise straws.